Inflammatory arthritis, which includes rheumatoid arthritis (RA), psoriatic arthritis (PsA), ankylosing spondylitis (AS) and other spondyloarthropathies, and juvenile inflammatory arthritis (JIA), typically does not interfere with pregnancy success. Most women deliver a healthy full-term baby. However, active arthritis does increase the risk for preterm birth and can cause the mother pain and disability.

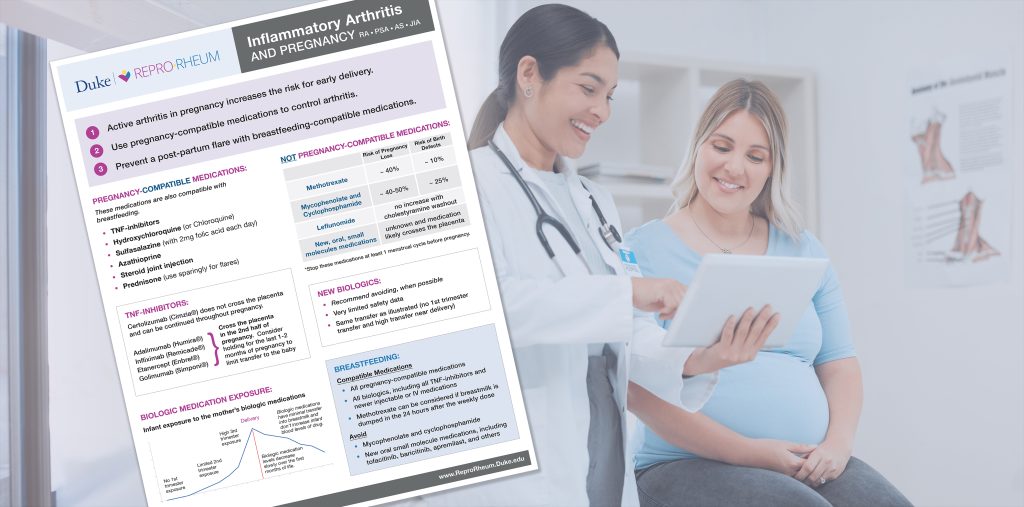
Checklist for Inflammatory Arthritis and Pregnancy
- Stop methotrexate and leflunomide prior to pregnancy
- Continue/start pregnancy-compatible medications to control arthritis
- Monitor arthritis activity in pregnancy
- Treat flares by adjusting medications, brief prednisone tapers, and/or joint injections
- Prevent post-partum flares with effective medication use soon after delivery
- Breastfeeding: nearly all anti-rheumatic medications are compatible with breastfeeding

Risks to Pregnancy
Women with active inflammatory arthritis during pregnancy have a higher rate of preterm delivery. While study results vary, an estimated 25% of pregnancies in women with active arthritis will deliver preterm, compared to fewer than 10% in women with inactive arthritis.
Pregnancy loss and preeclampsia are NOT increased in most women with inflammatory arthritis.

Arthritis Activity During and After Pregnancy
Arthritis symptoms may improve in some women but not all. Women who stop medications that were previously controlling their arthritis are likely to flare during pregnancy.
Post-partum flares are common in women who are not taking effective medications after delivery. These flares are often delayed by weeks or months after delivery, occurring once the mother’s immune system has returned to her baseline. This delay allows mothers to continue, increase, restart, or start medications to PREVENT a flare. Since almost all anti-rheumatic medications are compatible with breastfeeding, a mother does NOT need to choose between breastfeeding safely and treating her arthritis. Find breastfeeding-compatible medications here.

Pregnancy-Compatible Arthritis Medications
Use pregnancy-compatible medications to treat and prevent active arthritis. Some women may be able to taper their dose in pregnancy without a flare. A good goal is to take enough medication to avoid a flare that would require treatment with prednisone.
Medications that are not compatible with pregnancy should be replaced with one or more pregnancy-compatible medications to maintain control of arthritis during pregnancy:
Pregnancy-Compatible Medications
- TNF inhibitors – All are compatible with pregnancy. Certolizumab is the only one that does not transfer across the placenta in the 3rd trimester, so it can be continued throughout pregnancy. Consider holding other TNF-inhibitors several half-lives prior to expected delivery to limit transfer to the baby.
- Hydroxychloroquine or chloroquine
- Sulfasalazine – 2 mg of folic acid per day in pregnancy due to potential changes in folate metabolism.
- Azathioprine
- Steroid joint injections
- Prednisone (Used ONLY SPARINGLY, see below).
Special Considerations for Prednisone
Although prednisone is considered pregnancy-compatible, it is likely to be more dangerous than other pregnancy-compatible medications. Chronic and high doses of prednisone increase the risk for preterm delivery and decrease a baby’s birth weight.
- When possible, only use prednisone briefly for a flare.
- Replace prednisone with a pregnancy-compatible medication when possible.
- Steroid joint injections are safe in pregnancy and can be a good alternative to oral prednisone.

Arthritis Medications Incompatible with Pregnancy
Some arthritis medications can act as teratogens, or agents that can increase the risk of birth defects.
Methotrexate
Methotrexate is the most prescribed antirheumatic medication for inflammatory arthritis but is unfortunately also associated with pregnancy complications. With first trimester exposure to methotrexate in typically used doses, the risks of pregnancy loss doubles to about 40% and birth defects increase from 3% to 10% (Weber-Schoendorfer 2014). Stop methotrexate at least one menstrual cycle prior to trying to conceive.
If a mother is taking methotrexate at conception, she should stop the drug immediately and start taking folic acid 5 mg a day.
Leflunomide
When given to animals, leflunomide causes frequent pregnancy loss and birth defects. Fortunately, human data shows NO increase in pregnancy loss or birth defects in pregnancies conceived on leflunomide when women stop the drug at pregnancy discovery and complete a cholestyramine wash-out (Chambers 2010). All women should stop leflunomide prior to pregnancy. If their blood level of teriflunomide (leflunomide metabolite) is detectable, they should complete a cholestyramine washout procedure prior to trying to conceive (33 doses of 8g of cholestyramine spread over at least 11 days).
If a mother is taking leflunomide at conception, she should stop the drug immediately and start taking the cholestyramine wash-out.

Post-Partum Flares and Breastfeeding
Post-partum flares are common in women who are not taking effective medications after delivery. These flares are often delayed by weeks or months after delivery, occurring once the mother’s immune system has returned to her baseline. This delay allows mothers to continue, increase, restart, or start medications to PREVENT a flare. Since almost all anti-rheumatic medications are compatible with breastfeeding, a mother does NOT need to choose between breastfeeding safely and treating her arthritis.
Breastfeeding Compatible Arthritis Medications
- TNF inhibitors – All are compatible with breastfeeding
- Hydroxychloroquine or chloroquine
- Sulfasalazine
- Azathioprine
- Steroid joint injections
- Prednisone
- NSAIDS – Ibuprofen is preferred
- Any biologic medications – the large size of these molecules prevents significant transfer into breastmilk
Medications to Avoid with Breastfeeding
- Methotrexate – The ACR Reproductive Health Guidelines conditionally recommend against using methotrexate with breastfeeding. However, the blood and milk level of methotrexate is likely back to zero about 24 hours after the mother takes her weekly dose. For this reason, it could be safe to use with breastfeeding as long as the mother does not give the baby breastmilk produced in the 24 hours after her weekly methotrexate dose.
- Leflunomide – there is not sufficient data about transfer into breastmilk
- New small-molecule medications – the small size of these medications suggest they may transfer into breastmilk. The amount of transfer hasn’t been measured, so it is prudent to avoid these.

Antibody Testing for Connective Tissue Disease
Antibodies to RO/SSA
Women who have Rheumatoid Arthritis, Sjogren’s Syndrome, or have other signs of connective tissue disease should be tested for Ro/SSA and La/SSB antibodies prior to or early in pregnancy. If positive, regardless of the underlying rheumatic diagnosis, follow the Prevention, Monitoring, and Treatment guidance from the ACR Reproductive Health Guidelines.
Antiphospholipid Antibodies
Consider testing for antiphospholipid antibodies, especially if the mother has a history of pregnancy loss, premature delivery, and/or blood clotting. If positive, follow the ACR Reproductive Health Guidelines for management.

Internal Organ Disease
Sometimes women with inflammatory arthritis may have internal organ inflammation or damage. Depending on the severity and organ, this can increase the risks of pregnancy to both the baby and mother’s health. Consult with a Maternal-Fetal Medicine provider if the patient has moderate-to-severe heart, lung, or kidney disease.
Inflammatory Bowel Disease (IBD)
Both Crohn’s Disease and Ulcerative Colitis can flare during pregnancy and can be associated with higher rates of preterm birth and maternal harm. Work with a gastroenterologist and MFM to continue pregnancy-compatible medications to control IBD during pregnancy. Because of the severe impact of active IBD on the mother and her pregnancy, the continuation of TNF-inhibitors and newer biologics throughout pregnancy and delivery may be appropriate.