
Rheumatic Disease and Contraception
The American College of Rheumatology (ACR) recommends that patients with rheumatic disease use the most effective contraceptives that are safe for them in order to limit the risk posed by an unplanned pregnancy.
There are many factors to consider when choosing a form of contraception:
- The risks to the patient in pregnancy
- The risks to the baby from medications and rheumatic disease activity
- The medical risks of contraception (there are very few of these)
- The patient’s personal preference
Below, you will find information about different kinds of contraception, including long-acting reversible contraception (LARC), such as intrauterine devices (IUDs) and hormonal implants; permanent surgical contraceptive methods such as tubal ligation and vasectomy; and hormonal methods of contraception, including progesterone-only and progesterone-estrogen birth control pills, contraceptive rings, patches, and more. You will also find information about the benefits and risks associated with each method.
To learn more about each method, click on the plus sign for each category below.

Long-Acting Reversible Contraception (LARC)
Long-acting reversible contraception methods (LARC) include devices such as intrauterine devices (IUDs) and hormonal implants that are put in place by a health care provider. LARC are highly effective, highly recommended, and are safe for all patients with rheumatic disease. They are effective for several years until they are expired or are removed, require no pills or additional trips to the office or pharmacy, and are 20x more effective in preventing pregnancy than other contraceptives (Winner 2012).
Patients should be encouraged to use LARC to effectively delay or avoid pregnancy while on teratogenic medications, or if the patient is at high risk for pregnancy complications.
Intrauterine Device (IUD)
An intrauterine device (IUD) is small T-shaped device inserted into the uterus by a health care provider in a clinic. There are 2 types of IUD:
Copper IUD (ParaGard)
The copper IUD does not use hormones and can remain in place for up to 10 years. It does not change ovulation, won’t affect rheumatic disease, and won’t increase the risk of blood clots. The most common side effects are temporary pain when the IUD is first inserted. In some cases, a copper IUD increases menstrual bleeding.
Benefits
- More than 99% effective
- No impact on rheumatic disease
- Lasts up to 10 years
- No hormones
- No risk for blood clots
- No increased risk of infection
- Can be easily removed when ready for pregnancy
- Usually covered by insurance
Risks
- Temporary pain with placement
- Occasionally moves and causes pain
- Spotting in the first months after placement
- Can increase menstrual flow
- Does not protect against Sexually Transmitted Infection (STI)
Progesterone IUD
Mirena IUD, Skyla IUD, and others
There are multiple brands of progesterone IUDs. The most prescribed is called Mirena and is commonly used in adult patients. A smaller IUD, called Skyla, can also be used for teenage patients. These produce low and local levels of the hormone progesterone, which often prevents ovulation and prevents fertilization and pregnancy by changing the uterine lining and cervical fluids. Most patients have less menstrual flow with this type of IUD, and some patients stop menstruating entirely.
Benefits
- More than 99% effective
- No impact on rheumatic disease
- Lasts up to 5 years
- Often decreases menstrual flow
- No risk for blood clots
- No increased risk of infection
- Can be easily removed when ready for pregnancy
- Usually covered by insurance
Risks
- Temporary pain with placement
- Occasionally moves and causes pain
- Spotting in the first months after placement
- Does not protect against Sexually Transmitted Infection (STI)
Hormonal Implant
When a hormonal implant (Nexplanon®) is used, a health practitioner places a matchstick-sized (1.6 inches/4cm long) flexible plastic implant in the patient’s upper arm where it provides a continuous flow of low dose progesterone. This inhibits ovulation and changes the uterine lining and cervical fluids to prevent pregnancy.
Most patients have less menstrual flow with an implant. Implants can remain in place for years. The most common side effects are temporary pain and bruising when first inserted. Sometimes an implant can move, causing pain or mild local scarring. Spotting can also occur in the first months after placement.
Benefits
- More than 99% effective
- More effective than tubal ligation
- No impact on rheumatic disease
- Lasts 3-4 years
- Often decreases menstrual flow
- No risk for blood clots
- No increased risk of infection
- Can be easily removed when ready for pregnancy
- Usually covered by insurance
Risks
- Temporary pain or bruising with placement
- Occasionally moves and causes pain or mild local scarring
- Spotting in first months after placement
- Does not protect against STDs

Permanent Surgical Contraception
Vasectomy (for males) and tubal ligation or salpingectomy (for females) are all forms of surgical birth control. These are permanent and are 99% effective at preventing pregnancy, making them an excellent choice for people who are sure they do not ever want a pregnancy. While it may be possible to reverse a tubal ligation or vasectomy, doing so can be costly and may not be successful. For this reason, those who are unsure about whether they might want a pregnancy in the future should not pursue these options.
Tubal Ligation and Salpingectomy
Tubal ligation is a relatively minor surgical procedure done under anesthesia that blocks the fallopian tubes. There is a low, but real, risk for pregnancy after tubal ligation. Study results vary, but between 1-7% of women may become pregnant within the 5 years after a tubal ligation (Gariepy 2022) (Bouillon 2018). A salpingectomy, or removal of the tubes, is more effective, with a near-zero failure rate. Both procedures prevent eggs traveling from the ovary to the uterus. Tubal ligation or tube removal are most easily done during a caesarean section, if the patient and their obstetrician have agreed on this plan well in advance.
Benefits
- More than 99% effective (salpingectomy ONLY)
- No impact on rheumatic disease
- Permanent
- No hormones
- No risk for blood clots
- Usually covered by insurance
Risks
- Minor risks related to surgery
- Difficult to reverse
- Does not protect against Sexually Transmitted Infection (STI)
Vasectomy
A vasectomy is a minor surgical procedure undergone by a patient’s male partner, usually in an outpatient clinic, that ties off the vas deferens (the tube that carries sperm from the testes into the penis) so that sperm cannot enter the male’s ejaculate.
Benefits
- More than 99% effective
- No impact on rheumatic disease
- Permanent
- No hormones
- No risk for blood clots
- Usually covered by insurance
Risks
- Minor risks related to surgery
- Not effective in first 3 months after procedure (sperm count should be checked before having unprotected sex)
- Does not protect against Sexually Transmitted Disease (STI)
Hormonal Contraception
Hormonal birth control options must be obtained from a health care provider and/or pharmacy and taken on a regular schedule. Whether it includes progesterone alone or progesterone and estrogen, it works by inhibiting ovulation and changing the cervical and uterine fluids to prevent pregnancy. With perfect use, hormonal contraception is 99% effective, but in the real-world, about 4 to 9 of every 100 patients using hormonal contraception become pregnant in a year.
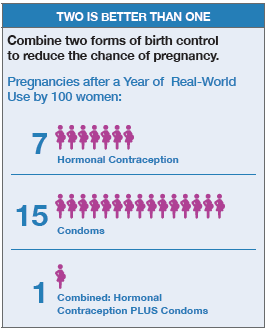
Two contraceptives are better than one
Hormonal contraception is less effective than what is theoretically possible because of everyday challenges of life, such as busy schedules, clinic hours, finances, insurance changes, or simply forgetting to take the contraception.
For this reason, patients should use a barrier method of contraception, such as condoms, spermicide, and/or a diaphragm in tandem with hormonal contraception to further decrease the risk of pregnancy, especially if the patient knows that they have missed or been late for a pill, shot, ring, or patch.
When hormonal contraception and barrier contraception methods are used in tandem, about 99% of pregnancies are prevented.
Limit menstrual bleeding with hormonal contraception: The use of a hormonal contraception method…
The use of a hormonal contraception method can decrease menstrual flow or, when active pills are used consecutively, menses can stop entirely. This can be particularly beneficial to patients with anemia as well as for women who prefer not to have a period. It is not medically necessary to have a menstrual period. For women who want to get pregnant in the future, menses will resume once contraception is discontinued.
Progesterone-Only Options
Progesterone-only contraception includes the “Mini Pill” and the “shot.” These methods are a good option for those at increased risk for blood clots, including women with antiphospholipid antibodies, or active lupus who are interested in hormonal birth control. (ACR Reproductive Health Guidelines 2020)
Progesterone-Only Pill (Mini Pill)
The mini pill will not increase the patient’s risk of blood clots but is the least effective hormonal contraception. To be effective, it must be taken at the same time every day. Being as little as 4 hours late in taking it could make it ineffective. This level of perfection taking a medication is impossible for most people. The mini pill is mostly used during breastfeeding, when ovulation is already less frequent. Encourage using a barrier method with the mini-pill to more effectively prevent pregnancy.
Benefits
- No impact on rheumatic disease
- Decreases menstrual flow
- No risk for blood clots
- Fertile soon after stopping
- Usually covered by insurance
Risks
- Pregnancy! 9 of every 100 patients will be pregnant within a year
- Less effective if one pill is taken just 4 hours late!
Injection: Medroxy-Progesterone (Depo-Provera®)
This progesterone-only shot is given every 12 weeks. It is typically injected deep into a muscle in a clinic. There is also an at-home subcutaneous (under the skin) injection available, but it is not used as often.
Benefits
- No impact on rheumatic disease
- Often decreases menstrual flow
- Usually covered by insurance
Risks
- 4 of every 100 patients using injection become pregnant in one year of real-world use
- Less effective if shots are received more than 12 weeks apart
- Bone loss with small increase in fragility fractures after 2 years of use (risk decreases once injections are stopped)
- Can take 6-12 months to regain fertility after stopping
- Mild weight gain (~5 pounds) due to increased appetite
- Not recommended for patients with antiphospholipid antibodies: May increase risk for blood clots
- Use some caution in patients with antiphospholipid antibodies: May increase risk for blood clots, though the evidence for this is evolving.
Estrogen-Containing Options
The hormone estrogen is included in oral birth control to make menstrual bleeding more predictable than with progesterone-only options. However, it can also increase the risk for blood clots in some people and may affect lupus activity. The ACR recommends that patients who have antiphospholipid antibodies and/or active lupus avoid using estrogen. (ACR Reproductive Health Guidelines 2020)
Combined Oral Contraceptive Pills (OCP)
The most prescribed birth control pills contain both estrogen and progesterone. They must be taken daily to be effective throughout the month. Typical pill packs come with 2 types of pills: active pills that contain both estrogen and progesterone, and placebo pills that do not contain hormones. For most patients, the bleeding of the menstrual cycle occurs during the week when placebo pills are taken.
The frequency of menstrual bleeding depends on the dosing pattern of combined OCP:
- Monthly menstrual cycles: 3 weeks of active pills followed by 1 week of placebo pills
- Quarterly menstrual cycles: 11 weeks of active pills followed by 1 weeks of placebo pills
- No menstrual cycles: Active pills are used continuously without placebo pills
Benefits
- No impact on most rheumatic diseases
- No impact on lupus activity in patients with stable lupus
- More predictable menstrual flow
- Often decreases menstrual flow
- Can stop menses entirely if taken continuously
- No effects on bone health
- Usually covered by insurance
Risks
- 7 of every 100 patients using OCP become pregnant in one year of real-world use
- Less effective if a pill is missed
- Not recommended for patients with antiphospholipid antibodies: May increase risk for blood clots
- Not recommended with severely active lupus
Contraceptive Ring
A flexible plastic ring that emits estrogen and progesterone is inserted into the vagina every month. Contraceptive rings contain estrogen and are not appropriate for patients with antiphospholipid antibodies or active lupus. The frequency of menstrual bleeding depends on the pattern of use. For most patients, a menstrual cycle typically occurs when the ring is removed for several days:
- Monthly menstrual cycles: 3 weeks with the ring in place, 1 week without it
- No menstrual cycles: 4 weeks with the ring in place, then replaced immediately
A new kind of ring may be soon available that can remain in place for a full year, preventing menstruation.
Benefits
- No impact on most rheumatic diseases
- No impact on lupus activity in patients with stable lupus
- More predictable menstrual flow
- Often decreases menstrual flow
- Can stop menses entirely if taken continuously
- No effect on bone health
- Usually covered by insurance
Risks
- 7 of every 100 patients using a contraceptive ring become pregnant in one year of real-world use
- Less effective if not changed on time
- Not recommended for patients with antiphospholipid antibodies: May increase risk for blood clots
- Not recommended with severely active lupus
Contraceptive Patch
The patch is a hormone emitting sticker that is placed on the skin for a week at a time. The patient has a menstrual period when they remove the patch for a week. The patch contains the highest amount of estrogen, so it is not appropriate for patients with antiphospholipid antibodies. The ACR also recommends avoiding the patch for ALL patients with systemic lupus, regardless of disease activity. (ACR Reproductive Health Guidelines 2020)
Benefits
- No impact on most rheumatic diseases
- More predictable menstrual flow
- Often decreases menstrual flow
- Can stop menses entirely if taken continuously
- No effect on bone health
- Usually covered by insurance
Risks
- 7 of every 100 patients using the contraceptive patch become pregnant in one year of real-world use
- Less effective if not replaced on time
- Not recommended for patients with antiphospholipid antibodies: May increase risk for blood clots
- Not recommended with lupus: Unknown impact on lupus activity

